This section of the website is to help people review their symptoms and self-determine if they might have AA. It also provides guidance to medical practitioners to make a clinical diagnosis of AA so treatment can get started as soon as possible. Previously, AA has been considered a hopeless, untreatable disease. This perception of AA is both outdated and no longer accurate. Today, AA can be specifically diagnosed and treated. The earlier in the AA disease process that both confirmation of an AA diagnosis is determined, and treatment is initiated, the better the potential for relief and hope for eventual recovery.
Special Note: To make a diagnosis of lumbar-sacral adhesive arachnoiditis, the patient should have a history of predisposing factors, typical symptoms, some physical abnormalities, and nerve root abnormalities on MRI. Laboratory testing may be normal, and MRI abnormalities, by themselves, are not sufficient for a diagnosis of adhesive arachnoiditis. In summary, adhesive arachnoiditis is a disease that is diagnosed when history, symptoms, physical findings, and MRI abnormalities are compatible.
Screening Test for Lumbar-Sacral Adhesive Arachnoiditis
Adhesive Arachnoiditis (AA) in the lumbar and/or sacral region of the spine is a condition that is the result of nerve roots adhering or gluing to the arachnoid layer of the spinal canal covering due to inflammation and adhesions. When this inflammatory process happens, a typical set of symptoms occurs which will both identify and separate the person with AA from those with back pain due to some other cause.
We have researched the symptoms of approximately 1000 people who have MRI-confirmed, lumbar-sacral AA. Over 80% have these five symptoms.
1. Constant back pain with stabbing or shooting pains into the buttocks, legs, or feet.
2. Pain is lessened by standing or reclining.
3. Difficulty starting, stopping, or holding urination.
4. Burning or electrical shocks in feet.
5. Sensation of insects or water on the legs.
If a person has 3 or more of the symptoms shown here, a contrast lumbar-sacral MRI and blood tests for spinal canal inflammation are warranted.
Cauda equina nerve roots, which number about a dozen, normally hang suspended in spinal fluid. They are in a symmetrical right to left pattern with equal numbers on each side.
AA occurs when a clump of nerve roots become attached by adhesions to the spinal canal covering that is composed of arachnoid and dural layers (meninges).
Here are AXIAL (head-to-toe) VIEWS of the Lumbar-Sacral Canal at about L4 – 5:
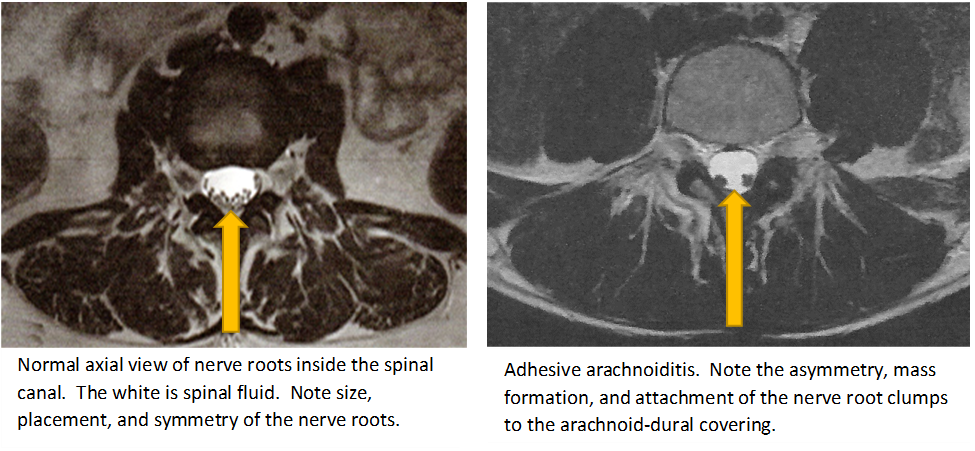
WHAT TO LOOK FOR: The arachnoid is the inner or middle layer of the spinal canal covering, scientifically called meninges or theca. The outer layer is the dura. On the axial MRI view, one is, therefore, primarily looking for a mass or clump of cauda equina nerve roots that are adhered or “stuck” to the covering by adhesions.
NOTE: MRI can be with or without contrast dye by use of new MRI techniques (e.g. Tesla).
AA typically appears as a darkened area in the lateral (sagittal) MRI view due to cauda equina nerve roots clumping together in an inflammatory, adhesive mass that obstructs spinal fluid flow.

Do You Have Neuroinflammation?
- Do you have periods of heat?
- Do you have periods of sweating?
- Do you feel like your body has too much electricity or “shock” at times?
- Do you have periods of burning in your feet, hands, pelvis, or buttocks?
- Do you have periods or episodes of strong feeling on your skin like bugs crawling or pin stabbing?
- Are you sensitive or become nauseated and dizzy in heat such as a hot summer day?
- Do the areas over pain sites sometimes become red and hot?
- Does your temperature rise at times?
- Are your pain flares accompanied by sweating and heat?
- Do you have periods of stabbing, shooting, or jerking pains?
- Do you have recurrent pain flares you can’t control?
If you answer yes to over half of the above questions, you will most likely need specific treatment for neuroinflammation.
The Cascade of Inflammation

Protruding discs are inflamed. They push on the dura-arachnoid covering of the spinal canal and inflammation spreads into the covering and nearby cauda equina nerve roots. Inflammation eventually produces adhesions which “glue” nerve roots together into an inflamed mass with imbedded nerve roots. The mass may later adhere or stick to the arachnoid-dural covering.
Time Frame and Process from Spinal Canal Puncture to AA
At least once a month we receive an urgent (often desperate) communication from a person who has begun to have some symptoms of AA (back pain, burning feet, headache, water sensation on skin, etc.) after a spinal tap, spinal anesthesia, or epidural injection for childbirth or therapy. In these cases, the unfortunate recipient has likely sustained a non-healing puncture of the arachnoid-dura (meninges/spinal canal covering). The puncture has inadvertently allowed a toxic contaminant (e.g. anesthesia) to enter the spinal fluid or has failed to close off and now has developed inflammation in the tissue around the open puncture. In almost all cases the person’s physicians initially believed that the headache and other symptoms would go away within a few days. This belief is justified since most puncture wounds will immediately heal and anesthetics and drugs that enter the spinal fluid will rapidly be eliminated.

THE PROCESS: In some cases, the puncture remains open and won’t rapidly heal and/or toxins that enter the spinal fluid don’t clear fast enough to prevent inflammation in cauda equina nerve roots. In these unfortunate cases, about 10 to 20 days pass and the persons symptoms have not abated. Physician and patient may jump to the erroneous conclusion that the symptoms are simply due to a spinal fluid leak. They don’t realize that an inflammatory process has begun. A blood patch is often given which, as often as not, causes an increase rather than a decrease in symptoms. About 20 to 30 days post-puncture, an MRI is typically done that is read as “normal” by the radiologist. The doctor then takes a “sigh of relief” and will likely tell the patient that nothing is seriously wrong.
FACTS: After a spinal canal puncture at least 60 to 90 days will elapse before AA shows on an MRI.
The pathologic process to develop AA is shown here. Aggressive treatment with corticosteroids and ketorolac are required at the onset of symptoms to hopefully prevent the development of AA. Do not delay as time is of the essence.
Categories of Severity
AA has different severities, and we divide the severity into 4 categories: (1) mild; (2) moderate; (3) severe; and (4) catastrophic. Below we list the categories with impairments and functions in each category. If you are in the mild or moderate category, you have an excellent chance of considerable recovery. In fact, you may not even require a prescription drug if you are in the mild category. If you are in the severe or catastrophic categories, you will need a full protocol with the most potent drugs, and you may even need an implanted electrical stimulator or intraspinal opioid pump to get adequate pain relief.
Stage One – Mild:
- Extremities: full range of motion, strength, extension
- No urinary or central symptoms*
- Normal ambulation
- Intermittent pain: non-opioid management is sufficient*
Stage Two – Moderate:
- Extremities: full range of motion, strength, extension
- Some urinary, gastrointestinal tract, and/or central symptoms*
- Normal ambulation
- Constant pain, but manageable without opioids
Stage Three – Severe:
- Extremities: some deficiency in range of motion, strength, extension
- Significant urinary, gastrointestinal tract, and/or central symptoms*
- Ambulates with assistance
- Severe, constant pain that requires daily opioids
Stage Four – Catastrophic:
- Extremities: significant deficiencies in range of motion, strength, or extension
- Significant urinary, gastrointestinal tract, or central symptoms*
- Bed bound part of each day
- Ambulation requires assistance
- Severe, intractable pain that requires palliative care
Notes on Interpretation
- Central refers to headaches, eye/ear/nasal symptoms such as blurred vision, tinnitus, vertigo, or nasal dripping
- Ambulation assistance means cane, walker, wheelchair
- MRI findings do not necessarily correlate with staging although the severe and catastrophic categories usually show one or more of these findings: dense scarring of nerve root clumps, multiple clumps, lower spinal canal distension (“empty sac”), peripheralization of nerve roots, calcification.
Note: Categories can overlap. Mild and moderate categories have the best potential for recovery which is motivation to diagnose AA and begin treatment as early as possible.
